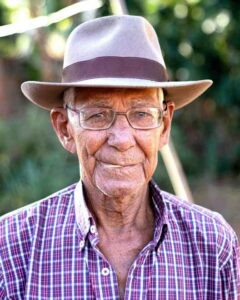
Identifying the Early Signs of Dementia
If you’re an older adult experiencing memory lapses, lack of focus or confusion — or you have a loved one with those symptoms, you may be concerned about the onset of dementia or Alzheimer’s disease. However, other treatable conditions can cause similar symptoms, and they can be easy for doctors to miss, says Ardeshir Hashmi, M.D., a geriatrician and section chief of Cleveland Clinic’s Center for Geriatric Medicine. There are clues that can help you in identifying the early signs of dementia.
“Sometimes there’s just a very superficial workup and then [the doctor says], ‘Here’s a pill for Alzheimer’s,’” Hashmi says. (While no drug has been proved to stop or slow the progression of dementia, there are several federally approved medications that can help manage the symptoms of Alzheimer’s.) “Before you make that conclusion, you should rule out all the other things that can be confused with dementia — things that are easily reversible.”
AARP’s recent article entitled “6 Medical Problems That Can Mimic Dementia — but Aren’t” identifies some common medical problems that can be mistaken for the early signs of dementia.
- Medication interactions or side effects. Older adults are more likely than younger people to develop cognitive impairment as a side effect of a medication. Drug toxicity is the reason in as many as 12% of patients who present with suspected dementia, research shows.
- A respiratory infection (including COVID-19). Any untreated infection can cause delirium — a sudden change in alertness, attention, memory and orientation that can mimic dementia. When you have an infection, the white blood cells in your body are sent to the infection site, causing a chemical change in the brain that makes some older adults feel drowsy, unfocused or confused. Respiratory infections are harder to diagnose in people over 65 because they are more likely to lack classic symptoms, such as a fever or a cough.
- A urinary tract infection (UTI). Research shows about 1 in 10 women older than 65 and up to 30% of women over 85 reported having had a urinary tract infection in the past year. Men are also more likely to experience UTIs as they age. However, most UTIs, and the accompanying cognitive issues, can be diagnosed with a simple urine test and then treated with an antibiotic.
- Sleep problems or disturbed sleep. If your sleep-wake cycle is disturbed or you have insomnia, you may experience dementia-like symptoms. These include trouble focusing, confusion, mental fatigue and irritability. Some older adults also suffer from sleep apnea, a sleep-related breathing problem that can deprive your brain of the oxygen it needs while you slumber, possibly causing long-term damage. Many seniors don’t realize they have this. Tell your doctor if you have signs of apnea, such as loud snoring, waking up gasping or choking, uncontrolled high blood pressure, a morning headache, or a dry mouth upon waking. If you are diagnosed with sleep apnea, using a continuous positive airway pressure machine (CPAP) while you snooze has been shown to be an effective treatment.
- Dehydration. If you take diuretics or laxatives, they can contribute to water loss. If you seem foggy or confused, see if your urine is dark yellow or brown, which can indicate a lack of fluids. Another sign of severe dehydration is a white coating on the tongue. To prevent dehydration, older adults should aim to get at least 48 ounces of caffeine-free fluids (six 8-ounce glasses) a day.
- Normal pressure hydrocephalus. This is a treatable disorder in which cerebrospinal fluid accumulates in the brain, disrupting and damaging nearby brain tissue and causing cognitive problems. A neurologist can diagnose normal pressure hydrocephalus using brain imaging and cerebrospinal fluid tests. It is treated by inserting a shunt into the brain to drain the fluid.
Know that dementia isn’t a normal expected part of aging. 11% of adults 65 and older have Alzheimer’s disease, the most common form of dementia. Identifying the early signs of dementia can dramatically increase the benefits of therapies and treatments. If you would like to learn more about dementia, and other related illnesses, please visit our previous posts.
Reference: AARP (March 21, 2022) “6 Medical Problems That Can Mimic Dementia — but Aren’t”
Photo by Mikhail Nilov